2024 Blue Care Network Annual Report: Transforming Faster for the Future

Blue Daily
| 5 min read

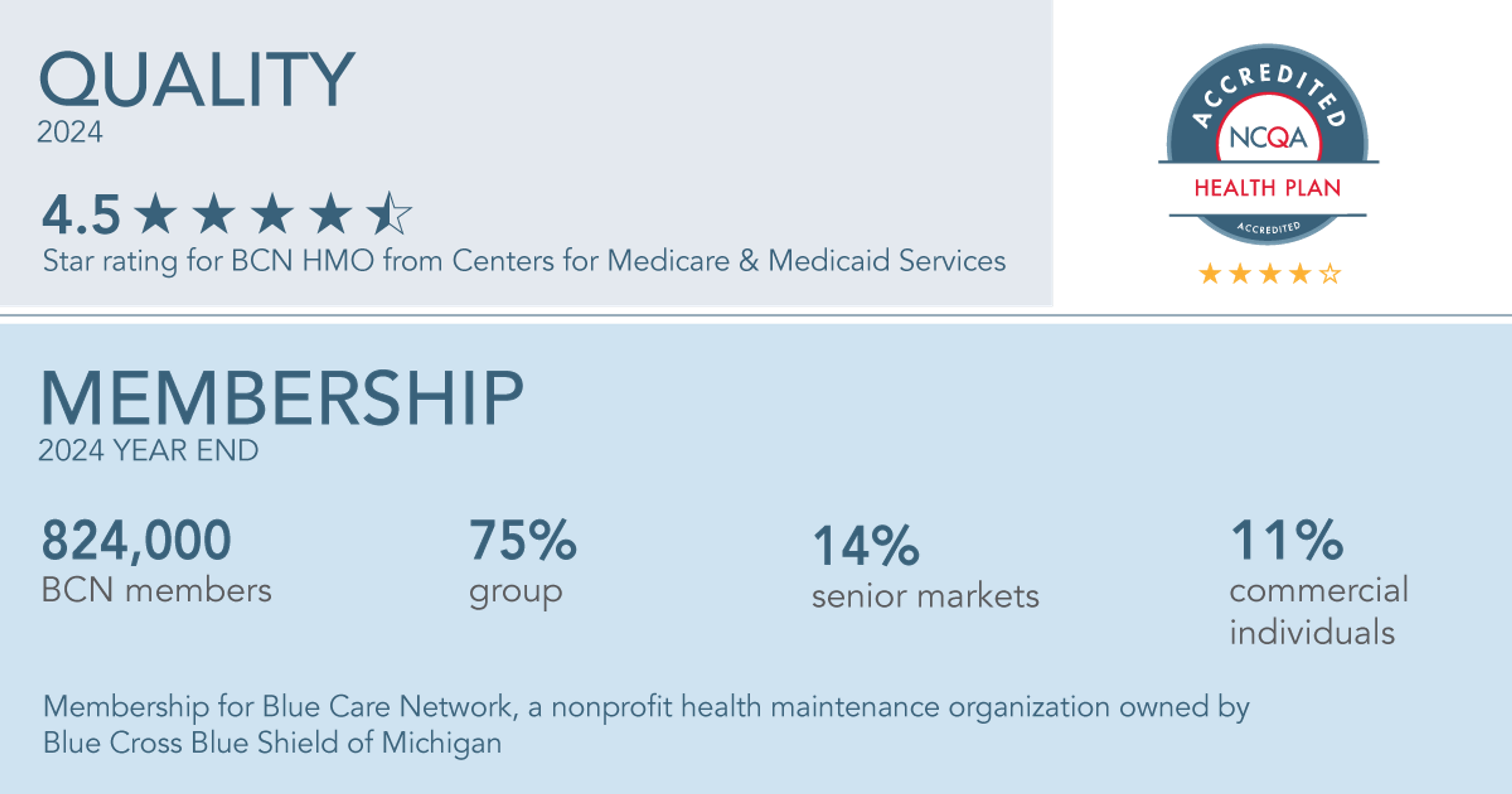
Blue Care Network is a nonprofit health maintenance organization owned by Blue Cross Blue Shield of Michigan. In 2024, BCN served nearly 824,000 members with access to care across all 83 counties in Michigan. Our annual report reveals how BCN contributes to our enterprise-wide endeavors to transform our operations and accelerate innovative solutions to make a healthier future for our members and customers.
“As the health care landscape continues to evolve, our direction is clear and full of opportunity. We will continue to advance our mission by delivering value to our members and helping shape a more affordable, effective health care system for the future.”
“At Blue Care Network, we put our members’ needs at the center of everything we do, focusing on personalized health care that impacts their whole health. And as we continuously adapt to the new and emerging needs of those we serve, we’re ready to help our customers meet the diverse health needs of their employees ― with coverage and options they can feel confident about, now and in the future.”
“Blue Care Network worked diligently during a financially challenging year to deliver quality and value in our products and programs. In service to our customers and members, we made sound decisions that helped control costs and remove barriers to accessing health care through value-based initiatives, our strong network of providers and utilization management strategies.”
A Year in Review: 2024 Highlights
At Blue Care Network, we believe we must transform faster to create a healthier future for the people who count on us. In 2024, we accelerated innovative solutions to expand access to care, to offer more affordable and convenient solutions ― and above all ― to improve the health of those we serve. Here are some highlights from last year that demonstrate how we’re evolving to meet the needs of our customers and members:
Adapting to meet the whole person health needs of our members
- Refreshed our Healthy Blue Living℠ HMO plan with our enhanced well-being services, including weight management and tobacco coaching programs, to empower members to achieve their health goals.
- Developed an app-based Virtual Muscle and Joint Health Program that helps eligible members prevent, treat and recover from muscle and joint pain through cutting-edge digital programs, personalized support and a holistic approach to managing musculoskeletal health.
- Added a comprehensive Cancer Support program through a virtual platform to give members with cancer and their caregivers access to educational resources, clinical oncology expertise, mental health support and a network of peer mentors.
- Helped eligible BCN members improve their psoriasis condition with a holistic home light therapy pilot program that helps them manage their symptoms with a portable phototherapy device, a convenient alternative to expensive specialty drug treatment; member satisfaction scores average a 4.7 out of 5 rating with a majority achieving clear skin or the ability to enter a maintenance phase to prevent future psoriasis flares.
Expanding access and affordability to improve health care delivery and value
- Developed Blue Elect Plus HRA℠ POS, a cost-effective plan solution that combines a health reimbursement arrangement with a point-of-service plan that offers provider choice and flexibility; because a health reimbursement arrangement is included, this plan can help members cover out-of-pocket costs.
- Launched 24/7 Virtual Care to provide members more access to medical and mental health through virtual visits with U.S. board-certified doctors and nurse practitioners.
- Helped BCN members access savings of more than $14 million in out-of-pocket costs through Price Edge, a service that finds the lowest price available on non-specialty, generic medications when members fill their prescriptions.
- Helped BCN members find manufacturer copayment assistance that saved them nearly $16 million in out-of-pocket costs, generating over $32 million in plan savings for group customers, on more than 300 specialty and other expensive medications with our High-Cost Drug Discount Optimization Program; the program recently expanded to include nearly 50 popular diabetes, cardiovascular and migraine drugs.
- Helped BCN members receive discounted rates on eligible medications through our Drug Adherence Discount Program and Generics Advantage Program.
Delivering a great experience for all
- Awarded a 4.5-star rating by the Centers for Medicare & Medicaid Services for the quality and performance of our BCN Advantage plans ― placing us among the highest-rated health plans in the country.
- Contributed to key initiatives that ranked Blue Cross Blue Shield of Michigan No. 1 in member satisfaction in the J.D. Power 2024 U.S. commercial member health plan study.
- Revitalized our well-being program with a digital platform that offers more personalization and an enhanced online experience to engage members in their health goals with Blue Cross Well-Being℠.
- Optimized our member account and mobile app experience with real-time prior authorization and referral notifications so members can track the status of their request to better manage their plan and avoid surprise out-of-pocket costs.
- Completed 141 virtual and in-person educational and open enrollment support sessions to help customers deliver better plan understanding to their members.
Read more about our enterprise-wide approach to delivering quality and value in the 2024 Blue Cross Blue Shield of Michigan Annual Report.